 Abraham Stroock '95 and his colleagues in tissue engineering aim to beat biology at its own game. It's the most common surgery in the United States: tympanostomy, in which children suffering from chronic ear infections have tubes inserted through their eardrums to drain fluid.
Abraham Stroock '95 and his colleagues in tissue engineering aim to beat biology at its own game. It's the most common surgery in the United States: tympanostomy, in which children suffering from chronic ear infections have tubes inserted through their eardrums to drain fluid.
Abraham Stroock '95 and his colleagues in tissue engineering aim to beat biology at its own game
It's the most common surgery in the United States: tympanostomy, in which children suffering from chronic ear infections have tubes inserted through their eardrums to drain fluid. "About a million kids a year get the operation, and it's wildly successful," says Cornell biomedical engineering professor Lawrence Bonassar. "People do it almost without a second thought. If your four-year-old has a series of ear infections, your pediatrician will say, 'This is what we have to do.'" But in as many as 10 percent of cases, the procedure results in a permanent hole in the eardrum—paradoxically providing an ideal passageway for infection. It's often repaired by taking a piece of cartilage from the outer ear and carving it into a dowel shape with flaps to adhere to the surrounding tissue. It's an imperfect solution; harvesting the cartilage requires general anesthesia and can be painful, and shaping the graft is time-consuming and therefore costly. But in his Grumman Hall lab, Bonassar has been working on an alternative—fabricating plugs of cartilage that surgeons can pop into place in a single step. The technology, under development by Memphis-based biotech firm Grace Medical, may have some initial safety tests in patients as soon as this spring; Bonassar and his colleagues have been collaborating with the company to translate their manufacturing processes to an industrial scale. "We're good at making a few dozen of these," he says, "but they need to make tens of thousands at a time."

Fashioning small bits of cartilage to address a complication from a routine pediatric surgery may not sound like a technological revolution. But as Assistant Professor Abraham Stroock '95 points out, high-profile breakthroughs in tissue engineering have been few and far between. A professor of chemical and biomolecular engineering, Stroock is one of the rising stars on Cornell's biomedical scene; last summer, MIT's Technology Review named him one of its 2007 Young Innovators, an honor given to scientists under thirty-five whose work the magazine finds most exciting. Sitting in his spacious office on the third floor of Olin Hall, Stroock lists what he sees as noteworthy advances in tissue engineering—inventions that have made it to clinical use in some form. He can tick them off on three fingers, each with metaphorical asterisks.

There's a product called Carticel, which Genzyme markets mostly to young people with knee injuries; surgeons send a sample of the patient's remaining healthy cartilage to the company, which grows it in culture to about 12 million cells and sends it back for implantation. "But it's not considered a large success," Stroock says. "People are often advised to get prosthetic knees instead." There's skin for burn patients or people with chronic wounds; doctors can send away cells from the patient and get back sheets of epithelium. "But it's in the early stages," he says, "and many surgeons still prefer to use grafts." And then there's an engineered extension for the bladder, designed by researchers at Wake Forest University for children suffering from a disease in which the organ fails to develop; it has been successfully implanted in patients and shown to grow along with them. Stroock says the technology, published in 2006 but not yet widely available, constitutes the field's "biggest success story so far."
Tissue work is just one part of the burgeoning field of biomedical engineering, but on the Hill it has been a focus of research and faculty hiring as the University expands its biomedical offerings. As Stroock puts it, "There are a lot of card-carrying tissue engineers on campus now." A gift from James Morgan '60, BME '62, MBA '63, and Rebecca Quinn Morgan '60 is funding collaborative research involving faculty from Engineering, Human Ecology, and the Medical college; projects have included research on biodegradable scaffolds for skin tissue by biomedical engineer Moonsoo Jin, fiber scientist C. C. Chu, and surgeon Roger Yurt, director of Weill Cornell's burn center.
Stroock stresses that tissue engineering is still in its infancy— or perhaps toddlerhood. Asked to name a benchmark for where the field stands, Stroock says, "We are definitely pre-integrated circuit—say, a stereo with vacuum tubes in it." The fundamental challenge, he notes, is that the "soft, organic, wet chemistries" that constitute life are tough to work with. In short: you can't make flesh out of glass. "When you think of regular engineering materials, you think of steel, you think of single-crystalline silicon," he says. "Biology does it almost exclusively with soft-gooey materials, and it turns out to be one of the significant challenges— how do you control a material that would like to turn into a puddle on the plate?" Another hurdle, he says, is the fact that living creatures are profoundly heterogeneous, with each building block having a distinct function. "We're not just uniform blobs stuck together," he says. "We have heterogeneity on all scales down to the molecular and cellular." As an example of how such variety affects clinical applications, he cites the repair of damaged cartilage, which often goes down to its junction with bone. "If you could hand the surgeon a plug that had both a seed of the cartilage and the bone, he could extract the damage and put it in," he says. "That would be a very valuable thing."
With the Vet college's Alan Nixon, Bonassar has been working to create such next-generation biological implants, coaxing bone-marrow-derived stem cells to become cartilage cells, which are then grown on tiny scaffolds that mimic the structural proteins found in the body. While medicine has been successful in restoring function to damaged or deteriorated joints with implants made of plastic and metal, Bonassar says, they have obvious limitations. "The properties of man-made materials change over time simply due to use, phenomena like fatigue and corrosion," he says. "That is why, if you have a bridge, you don't just let it sit there—you repaint it and repair the bolts, because they wear out. The unique thing about biological tissues is that they are constantly replacing themselves, constantly turning over and remodeling. And so by replacing bone with bone, you have a material that will maintain its properties over the long term."
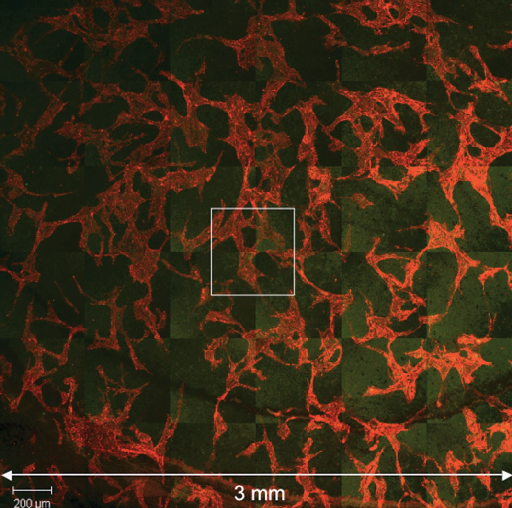
Stroock's biomedical work has been focused on the body's vascular system, which connects to his area of expertise: the field of microfluidics, in which fluids are manipulated at the colloidal scale, on the order of a micron and below. ("It's bigger than a molecule," he jokes, "smaller than a brick.") He has been exploring how to create microchips that mimic the vascular system— key to sustaining engineered tissue such as organs or muscle. Such devices, he says, could solve a fundamental problem. "If you want to make any human-scale piece of tissue, except maybe skin, the inevitable outcome is that if you have more than one layer of thickness, you have a region that is below the surface," he says. "If you feed oxygen and nutrients to the top, the region below becomes depleted, so you end up with a necrotic core—healthy tissue on the outside, but unhealthy or dead tissue in the center."
He's also interested in intercellular communication, understanding how cells send signals and organize themselves during development. "With an embryo, how does one side know that it's the left and the other side know that it's the right?" he asks. "Once you can't either tug on your neighbor or send him a chemical signal, how do you communicate on this larger scale?" The answer, he believes, is that a developing embryo forms a communication network analogous to those in human society—a hypothesis he hopes to use as a basis for engineering vascular tissue. "Once you're no longer just a clan and you become a village, you have to have paths to get from one place to another—you need an infrastructure for transport and communication, otherwise you'll decay back down to a clan," he explains. "So in the same sense, an embryo builds itself a rudimentary set of paths and they mature into a set of highways." And what Stroock calls his most exciting current work is a project he can only discuss in general terms because it's being reviewed for publication: inspired by a trip to Redwood National Park in Northern California, he has been exploring how trees move water from their roots to their leaves through capillary action. "It's extraordinary," he says. "All capillary action pulls from the top, so that means you're transmitting the force as a tension in the liquid. Trees use water like a very strong rope to pull more water up into themselves. This is a function that has never been captured in human technology."
The common denominator of Stroock's biomedical research is that by looking at biology through the eyes of an engineer, he can use the resulting insights to address the limitations of human physiology—be it a knee damaged in a basketball game or a liver failing due to hepatitis C. "Biology does many more interesting things on the micron scale than humans do," he says. "Right now we mostly shuttle electrons around, which is useful, and we all appreciate it in the form of computers and so on. But biology senses and generates forces, maintains life—so it sets up a career's worth of challenges." The field's blue-sky goal, he says, would be to engineer replacement parts for the human body: fully compatible organs, bone, skin, and more, potentially generated by a patient's own stem cells and therefore immune to rejection. "People still get replacement parts made of titanium and plastic, and not of themselves," Stroock says. "But in the coming decades, we could have replacement parts so when you get old, you don't just stay alive—you stay functional. And that is a beautiful challenge."
A Department of Their Own
Biomedical engineering hits its stride

Cornell has had a biomedical engineering department only since 2004, but it has already grown to comprise a professional master's program with some forty students, as well as a PhD program with more than fifty candidates. Among the fields where Cornell has the potential to be an international leader, department chairman Michael Shuler says, is cellular imaging; he cites the work of biomedical engineers Chris Schaffer and Warren Zipfel '87, PhD '93, and applied and engineering physicist Watt Webb in multiphoton microscopy and related technologies. "We're really interested in advanced imaging techniques that can be applied at the cellular molecular level," Shuler says. "Our overall philosophy—and a way we can somewhat separate ourselves from other departments—is that we're interested in understanding what happens at the molecular level and how it affects the cellular level, the tissue and organ levels, the physiology level. We want to go across those scales in a quantitative, predictive way."
Shuler himself has been working to create a "body on a chip," a tiny physical model of the body's systems and tissues that could play a vital role in drug evaluation. The chip, designed via mathematical modeling techniques, would have recirculating fluid that mimics the bloodstream. "Right now, you're looking at a cost on the order of $1 billion to develop a drug," he says. "Nine out of ten fail in medical trials. But if you could predict which of those are the most likely to be successful, it helps in two ways: you can eliminate your losers earlier, and you can design your clinical trials to identify potential problems earlier, so they don't pop up at the end and cause the product to fail after you've spent hundreds of millions of dollars." The project, also called a "mouse on a chip," could have the further benefit of reducing the need for laboratory animals—particularly important in Europe, where the use of animals in medical research is more strictly regulated.

Claudia Fischbach-Teschl joined the department after earning a PhD in pharmaceutical technology in her native Germany. Her research concentrates on cancer, including work with Weill Cornell neurosurgeon John Boockvar, MS '99, on a three-dimensional cell culture model for studying tumors, and studies on bone cancer metastasis with mechanical and aerospace engineering professor Marjolein van der Meulen. "It is a comparatively young field, which makes it exciting," Fischbach-Teschl says. "Everybody either has a background in something else and is excited about applying it to biological questions, or they're junior faculty who graduated in the field. There is huge potential, and the people in the field are truly engaged."
Although the University does not yet offer an undergraduate major in biomedical engineering, Shuler estimates that fifty to sixty BS students earn a minor each year. The department now has ten faculty, a number that Shuler hopes will grow to fifteen over the next four years. Their research is divided into five general areas: cellular imaging; micro-nano-biotechnology; biomaterials and drug development; molecular, cellular, and tissue engineering; and soft tissue biomechanics. The list underscores the multidisciplinary nature of the field, which can comprise everyone from physicists to computer scientists to mathematicians. "Biomedical engineering brings together biologists, electrical engineers, mechanical engineers, chemists, all sorts of sciences," says Valerie Cross, a PhD candidate under Stroock. "I think that's great, but it's also challenging, because of course I don't have expertise in all those areas. You have to work with lots of different people and also bridge the gap with the clinic."
The daughter of veterinarians, Cross once considered medical school; she says she was attracted to biomedical engineering because of the positive impact she can have on patients while staying on the technical side. She got first-hand exposure to the clinical world while working on Stroock's project on active wound dressings—spending weekends in Weill Cornell's burn unit, watching debridements and asking doctors and nurses about their equipment needs. "We can really advance medicine, not only for tissue engineering but in developing new tools, instrumentation, MRI machines," she says. "The whole field is exciting and growing fast."
Distance Learning
Can the 250 miles between Ithaca and the Medical college go from a burden to a blessing?
 Historically, universities with biomedical engineering departments have had medical schools close by; Johns Hopkins has long been top-ranked in the field. Cornell, of course, has Weill Cornell Medical College—but it's in Manhattan, 250 miles from Ithaca. Still, department chairman Michael Shuler says, "there is a lot of research we can do without the Medical college. We have the Vet college, which is really a second medical center, except the patients have four legs instead of two." Much of biomedical engineering professor Lawrence Bonassar's cartilage research, for example, has been done in collaboration with large animal surgery professor Alan Nixon, who works with bone-marrow-derived stem cells in horses.
Historically, universities with biomedical engineering departments have had medical schools close by; Johns Hopkins has long been top-ranked in the field. Cornell, of course, has Weill Cornell Medical College—but it's in Manhattan, 250 miles from Ithaca. Still, department chairman Michael Shuler says, "there is a lot of research we can do without the Medical college. We have the Vet college, which is really a second medical center, except the patients have four legs instead of two." Much of biomedical engineering professor Lawrence Bonassar's cartilage research, for example, has been done in collaboration with large animal surgery professor Alan Nixon, who works with bone-marrow-derived stem cells in horses.
But in the past few years—and especially since the arrival of President David Skorton, a cardiologist—the University has been promoting collaboration between the Ithaca and New York campuses, through financial and logistical support. Grant recipients include chemical and biomolecular engineering professor William Olbricht, who has been working with Weill Cornell faculty (including interventional neuroradiology director Pierre Gobin) to design a better microcatheter for inducing and treating strokes in lab rats. Ithaca-based biomedical engineer Abraham Stroock '95 worked with burn center director Roger Yurt and surgery professor Suzanne Schwartz to design an active wound dressing that could deliver drugs and serve as a diagnostic tool. And electrical and computer engineering professor Anthony Reeves has a long-standing collaboration with Weill Cornell radiologists Claudia Henschke and David Yankelevitz to develop technology—already licensed to General Electric—that interprets CT scans of the chest, helping doctors diagnose lung tumors.
To accustom biomedical engineering graduate students to the clinical world, the department requires PhD candidates to spend their first summer at Weill Cornell— living in medical student housing, shadowing a doctor, and conducting a small research project. "They gain quite a bit of maturity, and their confidence in working with physicians increases significantly," Shuler says. "The difference in sophistication that they have in medicine over that period of time is remarkable." The department's aim, Bonassar says, is to turn the distance problem on its head and make it into an advantage. Since the collaborating engineers and physicians often have to travel to each other's campuses—either for individual research projects or organized retreats—they tend to have each other's undivided attention. "I can't lie and say it wouldn't be wonderful if the medical school were in Ithaca," Bonassar says. "But in some ways the distance allows you to do things that you wouldn't be able to if the medical school was next door. When surgeons from Weill come up here, they are fully committed. If they came across the street, fitting us in between appointments, they'd be getting beeped all the time."


